A guest blog by Deborah P. Carey. Photo: Deborah at the New York City Marathon when her husband Jim ran the race to support LE&RN.
Why is yet another person telling their cancer story? These tales of how someone coped or didn’t cope with cancer tended to sound similar over time. Eighteen months ago, no amount of money would have pushed me to write about facing a cancer diagnosis. Today, I deeply hope that you find this piece to be uniquely informative and useful.
My story is not one of personal heroics in physical, mental, or spiritual ways. My intent is to suggest and promote action by and on behalf of cancer patients and medical professionals by sharing options for treatment that close friends provided for me. I didn’t realize going into this battle with cancer that, for me and many others, the hard work begins after surgery. That is when you are exposed to other medical issues and when you need to be or to find advocates to guide you on the recovery journey.
When you hear: "You definitely have cancer"
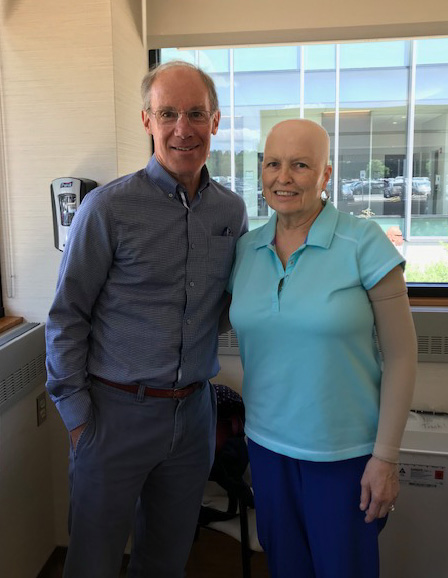 When you hear the words, “you definitely have cancer,” you may think you misheard the doctor. Like me, you ask your doctor if she or he said, “you do" or “you don’t “- an early form of denial. The ensuing walk through the dark forest of your worst fears and your search for some safe, steady path to take back to health and happier times is a personal challenge and, sometimes, a very lonely trip. (Deb is pictured at right with husband Jim.)
When you hear the words, “you definitely have cancer,” you may think you misheard the doctor. Like me, you ask your doctor if she or he said, “you do" or “you don’t “- an early form of denial. The ensuing walk through the dark forest of your worst fears and your search for some safe, steady path to take back to health and happier times is a personal challenge and, sometimes, a very lonely trip. (Deb is pictured at right with husband Jim.)
Even in the most supportive of relationships and medical settings, you may feel essentially alone because ultimately only you can choose how you will proceed emotionally, mentally, and spiritually. Doctors, families, friends, or online “experts” may offer a variety of directions to follow in dealing with your cancer. But you must decide the best ways to physically support and nurture yourself during the days and weeks ahead. The scariest feeling of all is helplessness.
Hearing a first-time diagnosis of breast cancer (confirmed as Stage 3C after surgery), I was shocked and confused, as well as scared. I had had annual mammograms, using the latest 3-D technology for the past two years, but this “invasive non-lobular cancer” was not picked up until it was a mass mandating a first-step mastectomy of my left breast. After telling my always-supportive husband, I thought about “who needs to know?” and created a shortlist of calls to place.
Reaching out for support
 One of those people was a close friend from our days at LeMoyne College, Bill Repicci (pictured with Deb and Jim at left), who heads the Lymphatic Education & Research Network (LE&RN), an organization committed to providing patient advocacy, research funding, and education for medical professionals, patients, and anyone interested in lymphedema and lymphatic diseases. I knew that the connections between cancer and the onset of lymphedema were quite common. I hoped that Bill could offer advice on dealing with doctors on how to address and possibly avoid any occurrence of this swelling.
One of those people was a close friend from our days at LeMoyne College, Bill Repicci (pictured with Deb and Jim at left), who heads the Lymphatic Education & Research Network (LE&RN), an organization committed to providing patient advocacy, research funding, and education for medical professionals, patients, and anyone interested in lymphedema and lymphatic diseases. I knew that the connections between cancer and the onset of lymphedema were quite common. I hoped that Bill could offer advice on dealing with doctors on how to address and possibly avoid any occurrence of this swelling.
He connected me with a surgeon at Memorial Sloan-Kettering Hospital in NYC. This doctor has multiple credentials in reconstructive, vascular, and plastic surgeries. His research area is lymphedema, which is the swelling that every patient with cancerous lymph nodes can fall victim to at any time post-surgery. Research and practice combined in his work to lead to a unique surgery that replaces cancerous lymph nodes with healthy ones transferred from the omentum, the area around the navel.
Unique to this surgery is the attachment of the nodes to the venous system for drainage. With an estimate of four to nine months or more before the transplanted nodes are established firmly enough to begin to work effectively, typical protocols for avoiding or handling early signs of lymphedema must be followed by his patients.
 My surgery, starting with the removal of all the left breast tissue while leaving intact blood vessels for the transplanting of belly tissue for reconstruction, and then the actual reconstructive process and lymphatic system transplantation and tie-in with intact veins, lasted a bit over 14 hours. Two specialists from Memorial Sloan Kettering, an excellent breast surgeon, and a leading reconstructive surgeon, worked on this process along with an assisting surgeon for the reconstructive process. (Photo at right: Dr. Anna Shapiro, my radiation oncologist from University Hospital Cancer Center at Upstate University Medical Center. Last day of radiation treatments- 28 and done!)
My surgery, starting with the removal of all the left breast tissue while leaving intact blood vessels for the transplanting of belly tissue for reconstruction, and then the actual reconstructive process and lymphatic system transplantation and tie-in with intact veins, lasted a bit over 14 hours. Two specialists from Memorial Sloan Kettering, an excellent breast surgeon, and a leading reconstructive surgeon, worked on this process along with an assisting surgeon for the reconstructive process. (Photo at right: Dr. Anna Shapiro, my radiation oncologist from University Hospital Cancer Center at Upstate University Medical Center. Last day of radiation treatments- 28 and done!)
I wore a compression sleeve, beginning shortly after surgery other than while sleeping, for several months. My newly placed nodes are now operative and, with the exception of short-term but still regular use of a compression sleeve, my left arm -- where part of 17 cancerous nodes were found -- is actually a bit smaller than my right!
A large part of my success in avoiding lymphedema was that I was assigned to a Certified Lymphedema Therapist, a doctorate in PT who immediately helped to explain why exercise, diet, and strategies such as lymphatic massage were critical to my recovery efforts. These actions could and should be known to all surgeons who work with patients likely to encounter swelling due to lymph node removal or damage. I’ve discovered since that many patients know nothing about the self-care actions that can be most beneficial in avoiding pain and infirmity after surgery.
We need to do better -- for all those dealing with cancer and lymphedema
 The point of my cancer story is that I had a connection with the doctors at Memorial Sloan-Kettering which very few cancer and/or lymphedema patients have available to them. That strikes me as unfair and very troubling. While my doctor has mentored “Fellows” - surgeons who are seeking advanced, specialized training in these areas, that is not a fast way to provide treatment to all those in need. (Photo at right: Deb's husband Jim running in the New York City Marathon in support of LE&RN.)
The point of my cancer story is that I had a connection with the doctors at Memorial Sloan-Kettering which very few cancer and/or lymphedema patients have available to them. That strikes me as unfair and very troubling. While my doctor has mentored “Fellows” - surgeons who are seeking advanced, specialized training in these areas, that is not a fast way to provide treatment to all those in need. (Photo at right: Deb's husband Jim running in the New York City Marathon in support of LE&RN.)
In order to handle the demands of this training, especially in costly cities such as NYC, doctors who would like to develop their skills for doing this surgery need compensation to cover the cost of living every day - food, housing, transportation, heat, etc. Hospitals need to be able to attract surgeons who have demonstrated surgical skills and stamina needed to handle the extremely delicate nature of working with the lymphatic system, nerves, veins, and blood vessels in what can be a very lengthy surgical procedure.
However, one must be aware that particular surgery is not sufficient to address the needs of current or future lymphedema sufferers. Research is ongoing on new, possible, and current strategies, and information must be easily and broadly disseminated so we learn more about these diseases/disorders, and can take the best action to help us cope and heal.
 Shortly after receiving my diagnosis and the news that a mastectomy would be the first step in treating this cancer, I began walking daily in a form of meditation and prayer. I urgently needed to find both the spiritual and emotional strength to cope with all that awaited.
Shortly after receiving my diagnosis and the news that a mastectomy would be the first step in treating this cancer, I began walking daily in a form of meditation and prayer. I urgently needed to find both the spiritual and emotional strength to cope with all that awaited.
Of course, I questioned “Why me?” and “Why now?” and “How could this happen when I am checked every year?” But those questions don’t lead to answers very easily. It is very important to have support, care, and most importantly, the medical attention you deserve and need to assure you that everything will be addressed effectively and efficiently.
In my situation, I relied on my strong spiritual belief that everything happens for reasons often unknown to us, but ultimately “right” even when contrary to our immediate wants and needs. My wonderful support crew of family, friends, along with fellow patients and survivors, truly provided a sense of being uplifted and loved, above the negative feelings and fears. But not everyone has these types of resources.
Public health clinicians and the medical community in general are not always aware of the extent that lymphedema and lymphatic diseases can extensively affect someone’s quality of health. One must know that their medical team has the knowledge and skills to help them to heal as thoroughly as possible because the team knows that the cancer patient may well face additional battles after surgery.
Lymphedema training in the medical community
 In my journey through four medical settings for surgery, chemotherapy, radiation, and cancer rehabilitation (physically therapy), I have asked doctors, nurses, and support personnel if they were trained to deal with lymphedema. I volunteer in a local hospital and could ask professionals about their educational experiences. Most who I asked in my upstate NY area had no training with lymphedema, or perhaps were given a 15-20 minute exposure to the topic in a related subject lecture. These responses are not solely heard in my part of the country! Some professionals in the relevant medical fields struggle to recall their medical school education, if any, about lymphedema. Many breast cancer survivors have shared with me that they have not heard about lymphedema or about wearing compression sleeves when traveling by air or for other purposes relevant to possibly affecting their surgical areas. (Photo: Deb at the New York City Marathon with a friend.)
In my journey through four medical settings for surgery, chemotherapy, radiation, and cancer rehabilitation (physically therapy), I have asked doctors, nurses, and support personnel if they were trained to deal with lymphedema. I volunteer in a local hospital and could ask professionals about their educational experiences. Most who I asked in my upstate NY area had no training with lymphedema, or perhaps were given a 15-20 minute exposure to the topic in a related subject lecture. These responses are not solely heard in my part of the country! Some professionals in the relevant medical fields struggle to recall their medical school education, if any, about lymphedema. Many breast cancer survivors have shared with me that they have not heard about lymphedema or about wearing compression sleeves when traveling by air or for other purposes relevant to possibly affecting their surgical areas. (Photo: Deb at the New York City Marathon with a friend.)
Many men use compression garments to handle lymphedema subsequent to surgeries that lead to leg swelling. Male friends who asked why I wore the sleeve when golfing commented to me that they’ve seen guys wearing them on their legs but thought it was a varicose vein issue. One personal friend who fought breast cancer for nine incredibly brave years told me that the only comment she received from a medical professional was that she should buy a sleeve and wear it on the arm closest to her surgery site so she “wouldn’t swell up.” That was it.
 I do not know “why me” or “why now” to the extent I hope I might in my next life, but it became clear to me that my experience provides an opportunity to advocate for others who might not know about or have the means to explore information on their original diagnosis or what to expect from their medical care providers. This “story” has become a responsibility for me, and these critical points must become part of your responsibility for your own well-being:
I do not know “why me” or “why now” to the extent I hope I might in my next life, but it became clear to me that my experience provides an opportunity to advocate for others who might not know about or have the means to explore information on their original diagnosis or what to expect from their medical care providers. This “story” has become a responsibility for me, and these critical points must become part of your responsibility for your own well-being:
- Get regular medical checkups, especially if there is any history of cancer in your background. Look for local free or reduced price/sliding scale clinics in your area if you do not have insurance coverage for these checkups.
- Go to the doctor’s office/clinic/hospital with a list of your questions and worries. Be insistent that you need enough information to understand what is happening to you now and in the near future.
- Ask your surgeon what he/she can tell you about lymphedema, including how likely you might be to develop it post-surgery. Ask where you can go for further information, and also ask who on the health care team will help you to learn self-care for minimizing the possibility of lymphedema now or if it occurs down the road.
- Ask who provides physical therapy after your surgery, and check whether that individual has been certified in lymphedema therapy. Go to all appointments with this therapist!
- Seek information online, ask the doctors for any printed materials about handling your cancer and treatments, and always visit the doctor with written notes on any questions that occur to you between appointments.
- Look up organizations such as the Lymphatic Education and Research Network (LE&RN), led by my friend Bill Repicci, that can help provide patient-focused information for you. The American Cancer Society has free information and services to assist you as well. Never be afraid to speak to other patients in offices. We are all part of each other’s networks!
Remember that you are not alone in this journey through your disease to better health. Many of us think about all of you and send our prayers, positive thoughts, good vibes, and hopes for healing, that each and every one of you gets the best care and the best outcomes on your particular paths. Most importantly, be your own best resource and advocate, while also valuing all those who contribute to your well-being in any possible way. Speak up, speak out, and share your stories -- this makes cancer less frightening and lymphedema less likely!
Oh - and thank you for reading this cancer story!
