New Science and Lymphedema, by Dr. Andrea Brennan, OTR/L, CLT-LANA, WCC
Thinking Lymphatically: Microvascular Fluid Exchange
New research is proving that it’s crucial to have a lymphatic-first mindset. Why? Because all edema is lymphatic overload - a fact that phlebologists and other medical practitioners learn in their training, but isn’t emphasized in mainstream medical education.
To fully understand lymphatic overload, let’s go back to the basics. If we are going to talk about chronic edema and lymphedema, first we must understand the dynamics of microvascular fluid exchange.
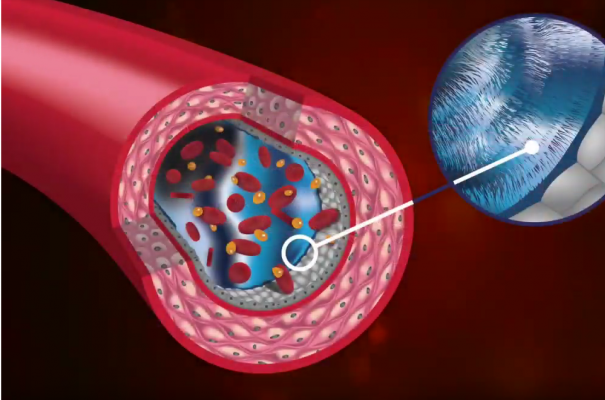
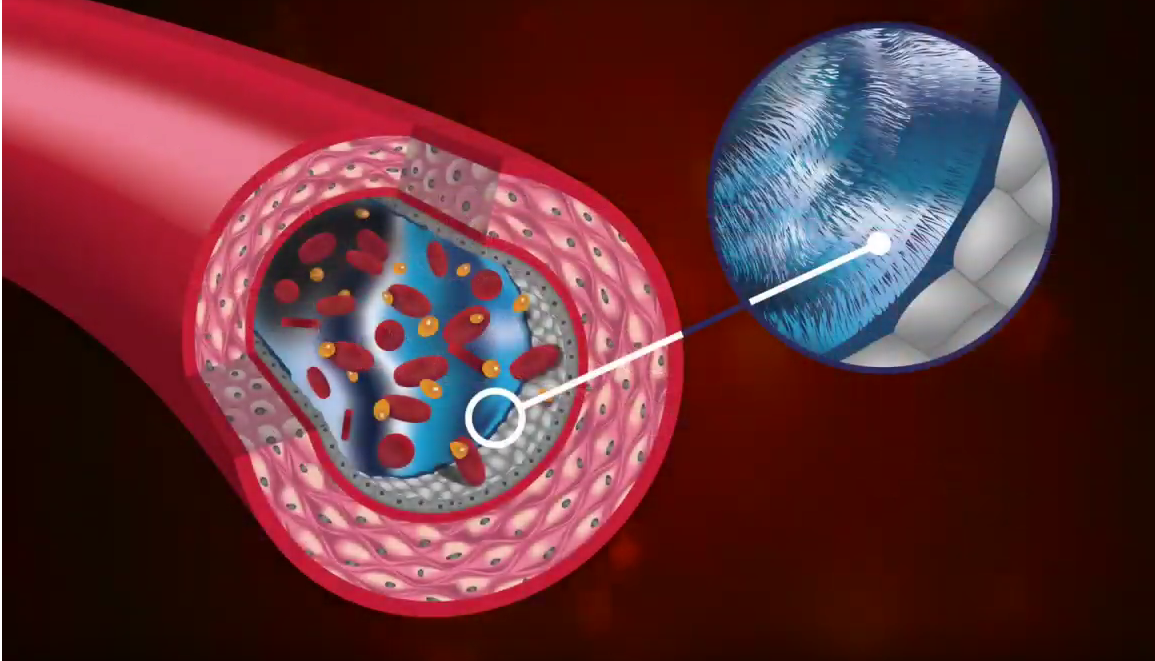
Within microvascular fluid exchange, there are four components: capillaries, tissue channels, proteolytic cells (or macrophages), and initial lymphatics. The capillaries have different thicknesses and holes - called fenestrations - which allow fluid and protein to leave the bloodstream.
Between the capillaries and lymphatics is the interstitial fluid. In the channels of this interstitial fluid there are macrophages, collagen, proteins - all kinds of energy molecules and fluid. Macrophages linger in these channels, breaking down larger particles in preparation for entering the lymphatic system. The particles are quite large - too large, in fact, to enter the lymphatics.
This is the process of microvascular fluid exchange, and within it lies our central problem: large amounts of cellular debris must be broken down, or otherwise pressure begins to build.
The Starling Principle vs. New Research
It’s all about pressure. The pressures in microvascular fluid exchange are like a garden hose. When you turn on the hose, the water goes from the area of high pressure over to the area of low pressure.
These pressures, where fluid is moving on a microvascular level as it approaches the lymphatic system, were the focus of Ernest Starling’s famous research in 1896. He studied the capillaries and interstitial fluid to understand the processes of absorption and filtration.
And that’s where Ernest Starling was brilliant. He came up with the principle that these capillaries, which are semi-permeable, transfer fluid by filtration. In other words, fluid can cross the capillary wall and bring cellular debris. That happens because there is pressure along the capillary wall.
Starling’s findings lasted more than 100 years, until the advent of electron microscopy and new ways to assess microcirculation. With today’s technology, scientists are able to measure the various pressures with much more precision. What they have found is that Starling was quite right - but he forgot to take into consideration some of the other pressures in the interstitium.
This brings us to new research by J.R. Levick and C.C. Michel, who have found that there is a lining in the capillary wall called the endothelial glycocalyx. These hairlike structures create an exclusion zone, where permeability is reduced.
Fluid can’t go backward, so where does it go? It has to go somewhere. Otherwise, the person would swell like a balloon.
This is the primary point where Starling differs from Levick and Michel: permeability. The discovery of the glycocalyx has changed our understanding of microvascular fluid exchange.
The latest research integrates new physiological findings with Starling’s model. The glycocalyx is hydrophobic and prevents the reabsorption of fluid into the venule. What does that mean? It’s significant. Because where does that fluid go? If not into the venous side, where else?
This new research shows that in terms of the fluid that crosses into interstitium, essentially 100% flows into the lymphatic system. There is no reabsorption into the venous side, in normal situations. It is, in fact, the lymphatic system that is responsible for absorption of excess fluids in the interstitium.
Clinical Implications for Doctors and Patients
Clinical practitioners who treat edema should pay close attention to what this microvascular fluid research means for their day-to-day patient care.
We are looking at an important new concept because of its clinical implications. This concept, which is an updated look of the original Starling principle, makes an enormous contribution to our understanding of edema. As of yet, it is not in mainstream medical education.
Here are some of the most important implications for patient care.
Keep in mind that it’s all about pressure and finding equilibrium, also known as osmotic asymmetry. When you think of it this way, it’s easier to understand persistent problems with the transfer of fluids within the circulatory system.
Improvements in lymphatic flow should be one of the first considerations for treatment of all peripheral edema.
Remember that all chronic peripheral edema is due to lymphatic overload.
Just because someone has edema does not mean they have lymphedema. However, edema left unchecked will eventually become lymphedema.
Early treatment is extremely important, because it prevents the advancement of disease.
Many of your patients with the most serious lymphatic issues have likely seen other medical practitioners in the past, and have remained undiagnosed, causing significant delays in treatment.
Have You Seen This Patient?
In my interactions with lymphedema patients, I see scenarios you would likely recognize in your own patients. I’ve seen people with the earliest stages of edema, and I’ve seen some of the toughest, most neglected, most treatment-resistant chronic lymphedema cases.
Unfortunately, many of these patients have been trying to find adequate treatment for months or even years. These are people who are suffering. These people need our help.
Below, you can see photos that show lymphedema and related problems. If you see patients with issues like these, they urgently need medical assistance. Embrace the new science of lymphedema and put this knowledge to good use in your practice.


Photos used with permission.
Next up in the Think Lymphatically Series, we’ll go deeper into the Starling principle and the importance of understanding the role of the glycocalyx in microvascular fluid exchange.
About The Author
Dr. Andrea Brennan, OTD, OTR/L, CLT-LANA, CI-CS, WCC holds a clinical doctorate in occupational therapy with a specialty in lymphedema practice management. She has been in the field for more than 35 years and has spent the past 20 years specializing in lymphedema diagnosis and treatment.