A guest blog post by Melissa B. Aldrich, M.B.A., Ph.D. This is the second article in a two-part series about Dr. Aldrich and her colleagues’ clinical imaging studies and emerging research into the development of lymphedema. It’s a 7-minute read.
I am part of a team of immunologists, biomedical engineers, biologists, and chemists working on pre-clinical and clinical imaging studies of breast cancer-related lymphedema (BCRL), lipedema, and lymphatics in the setting of cancer, in collaboration with physicians and therapists. The imaging modality developed and utilized by our group is near-infrared fluorescence lymphatic imaging (NIRF-LI), that allows us to “see through the skin” and observe nearly real-time lymphatic pumping. Two of our current clinical studies include a longitudinal breast cancer-related lymphedema (BCRL) imaging study and another study investigating lymphatic microsurgeries.
Ultimately, the goal of our research is to improve patient outcomes for those with lymphedema. As a disclaimer, I state that I am not a physician, and do not claim to recommend any particular treatment for any medical condition. In this article, I’d like to share tidbits from our, and other groups’, research that hint at possible effects of exercise on lymphedema, and the value of imaging lymphatics for directing therapy.
Can Exercise Promote Lymphatic Function?
Published research studies from other research groups of exercise and lymphedema have transitioned in recent years from determining whether carefully prescribed exercise is safe, to showing that it is beneficial [1].
In a past clinical study, we imaged an elderly woman who loved to dance for ~12 hours every weekend. She had avoided development of lymphedema, despite three rounds of different cancers with extensive lymph node removal. Did her dancing stimulate lymph flow, perhaps promote connections of surgery-severed lymphatics to draining lymphatic and venous vessels, and deter lymphedema?
We know that doxorubicin, an anthracycline antibiotic with cancer-fighting benefits, commonly used in cancer patients, can kill heart muscle cells [2]. In mouse studies, these muscle cells around the heart vessels seem to be better-preserved in mice who exercise regularly [3]. A recent study showed that doxorubicin has a detrimental effect on lymphatic pumping [4]. Does doxorubicin also kill the muscle cells surrounding collector lymphatic vessels, and could exercise override such an effect?
Exercise decreases chronic “bad” inflammation that wreaks havoc on the body. We have shown in mouse studies that some inflammatory molecules can stop lymphatic pumping [5]--could exercise counteract such inflammation and allow lymphatic pumping to resume?
For those who can’t exercise due to mobility issues or other concerns, perhaps deep breathing may be helpful. Last December during a “show and tell” lymphatic imaging event, I watched as deep breathing appeared to stimulate lymphatic pulsing, which came as a total surprise to myself and the audience and to me.
Are there neurological circuits controlling lymph pumping that can be “fired up” by deep breaths? Imagine the prospect of helping lymphedema patients improve their health outcomes simply by beginning a regimen of daily exercise and deep breathing. Perhaps future research will provide more answers.
The Value of Imaging Lymphatics
Now let’s shift to a crucial tool for diagnosing lymphedema and potentially directing better treatment outcomes: imaging. NIRF-LI allows us to “see through the skin” to observe whether lymph is pumping normally. Other clinical and investigational lymphatic imaging tools, that do not show on-the-spot, real-time pumping, but do provide indirect pumping and lymphatic vessel anatomy information, include lymphoscintigraphy, magnetic resonance lymphography (MRL), single-photon emission computerized tomography (SPECT-CT), and photoacoustic tomography.
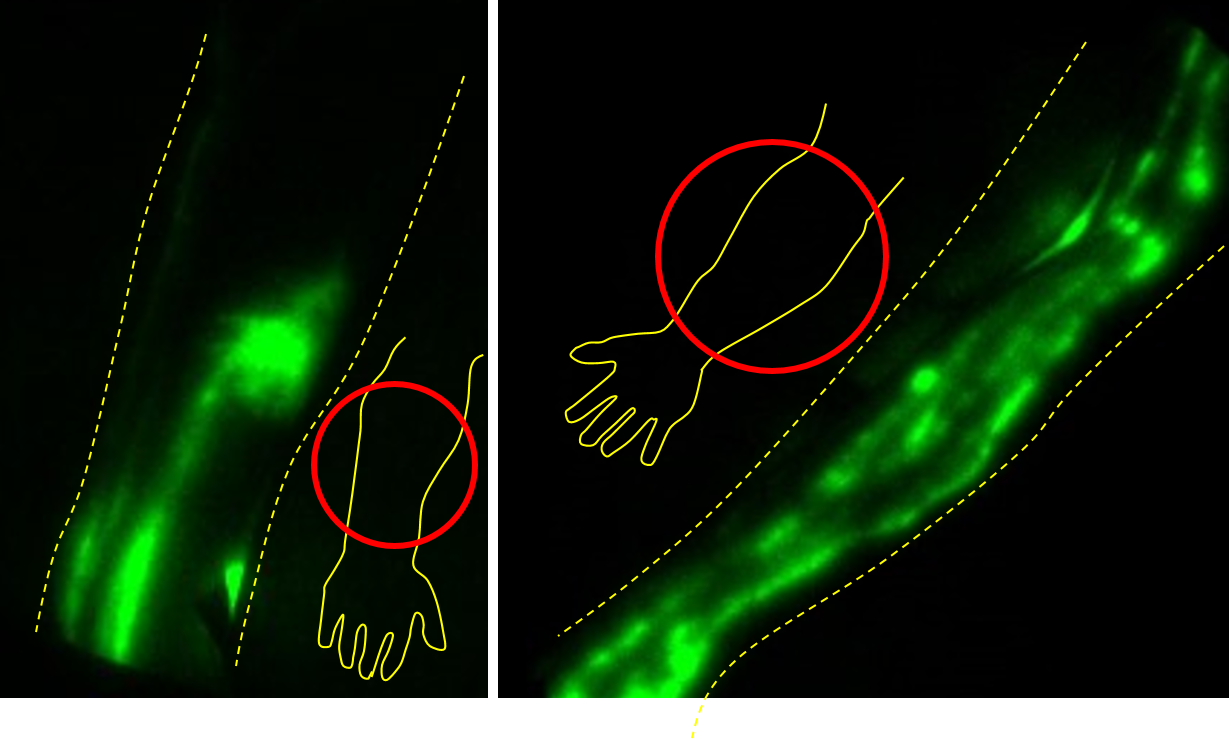 In these NIRF-LI images above, abnormal lymphatic backflow appears as a disorganized, blurry area in an arm (left image), while normal lymphatic vessels are linear, and actively pulse lymph (right image).
In these NIRF-LI images above, abnormal lymphatic backflow appears as a disorganized, blurry area in an arm (left image), while normal lymphatic vessels are linear, and actively pulse lymph (right image).
Lymphatic imaging can show whether or not lymphedema treatment is warranted. In a previously mentioned case, the elderly, dancing “party girl,” who had no lymphedema but would ordinarily have been considered high-risk for developing BCRL, could have received needless prophylactic treatment. In another case, NIRF-LI showed lymphatic backflow, a hallmark of lymphedema, in a breast cancer patient when imaged 6 months after axillary lymph node dissection (ALND) and radiation therapy (RT). She started exercising and using compression, and at 12 months and 18 months later, the backflow was gone. She had no arm swelling when the backflow was first spotted, but the imaging alerted her to developing lymphatic dysfunction, and her early compression and exercise may have allowed her to avoid BCRL.
Some of our BCRL study subjects display at least partially dysfunctional lymphatics before ALND and RT. Seeing problematic lymphatics early can allow the oncologist to refer patients for lymphedema treatment before tell-tale swelling sets in later, and lymphatic damage may have progressed. In cases of primary lymphedema and vascular anomalies, as well as congenital conditions with associated lymphedema, NIRF-LI can guide therapists’ massage efforts and compression recommendations, by showing if and where there are functional, pumping lymphatics.
NIRF-LI can help with the assessment of nonsurgical and surgical treatment options for lymphedema, lipedema, and lymphatic malformations [6]. It has also been beneficial in assessing treatments for vascular diseases such as chronic venous insufficiency and peripheral arterial disease [7].
NIRF-LI can even help us inspect and protect the brain. Brain waste fluid drainage moves through the glymphatics, a recently re-discovered system of perivascular tunnels that clears waste from the central nervous system [8]. Using NIRF-LI, doctors can visualize cerebral spinal fluid movement as it moves out of the brain through the cervical/neck lymph nodes [9].
We have learned that drainage through the glymphatics speeds up when we sleep, perhaps clearing amyloid plaques and inflammatory agents from the brain [10]. Since bad sleep is suspected to contribute to the development of Alzheimer’s disease, imaging of glymphatic drainage could provide information to guide early Alzheimer’s diagnosis and treatment.
Making Good Use of Lymphedema Treatment Tools
In summary, research is showing that exercise may hold benefits for people with lymphedema, and perhaps should be considered when developing therapeutic plans. Deep breathing may deserve investigation as a lymphedema treatment tool, as well.
NIRF-LI is providing a wealth of information that supports detection at the earliest stages of lymph dysfunction, allowing intervention as soon as possible, and improvement of long-term health.
I look forward to continuing my team’s current and ongoing studies of lymphatics and sharing these promising findings with other lymphatic researchers, medical professionals, and lymphedema patients.
About Dr. Aldrich
Melissa Aldrich, M.B.A., Ph. D is an immunologist who works as part of a team of biomedical engineers, biologists, and other professionals who are investigating lymphatics in a variety of contexts. Dr. Aldrich received her B.A. in Biochemistry from the University of Texas-Austin, her M.B.A. from the University of Houston, and Ph.D. in Immunology from the University of Texas Health Science Center/M.D. Anderson Cancer Center Graduate School of Biomedical Sciences in Houston, focusing on severe combined immune deficiency. Currently, Dr. Aldrich is leading a five-year NIH-funded study of breast cancer patients who are at high risk of immunological changes and the development of lymphedema, and a new three-year study of lymphatic microsurgeries. Click here to see more about her background and credentials.
References
Morris C, Wonders KY. Concise review on the safety of exercise on symptoms of lymphedema. World J Clin Oncol 2015 10, 43-44. doi: 10.5306/wjco.v6.i4.43
Cappetta D, De Angelis A, Sapio L, Prezioso L, Illiano M, Quaini F, Rossi F, Berrino L, Naviglio S, Urbanek K. Oxidative stress and cellular response to doxorubicin: a common factor in the complex milieu of anthracycline cardiotoxicity. Oxid Med Cell Longev 2017 2017,1521020. doi: 10.115/2017/1521020
Wang F, Iskra B, Kleinerman E, Alvarez-Florez C, Andrews T, Shaw A, Chandra J, Schadler K, Aune GJ. Aerobic exercise during early murine doxorubicin exposure mitigates cardiac toxicity. J Pediatr Hematol Oncol 2018 40, 2018-215. doi: 10.1097/MPH.0000000000001112
Stolarz AJ, Sarimollaoglu M, Marecki JC, Fletcher TW, Galanzha EI, Rhee SW, Zharov VP, Klimberg VS, Rusch NJ. Doxorubicin activates ryanodine receptors in rat lymphatic muscle cells to attenuate rhythmic contractions and lymph flow. J Pharmacol Exp Ther 2019 371, 278-289. doi: 10.1124/jpet.119.257592
Aldrich MB, Sevick-Muraca EM. Cytokines are systemic effectors of lymphatic function in acute inflammation. Cytokine 2013 64, 362-369. doi: 10.1016/j.cyto.2013.05.015
Rasmussen JC, Zvavanjanja RC, Aldrich MB, Greives MR, Sevick-Muraca EM. Near-infrared fluorescence lymphatic imaging of Klippel-Trenaunay syndrome. J Vasc Surg Venous Lymphat Disord 2017 5, 533-537. doi: 10.1016/j.jvsv.2017.011
Rasmussen JC, et al. Degradation of lymphatic anatomy and function in early venous insufficiency. Under review.
Plog BA, Nedergaard. The glymphatic system in central nervous system health and disease: past, present, and future. Annu Rev Pathol 2018 13, 379-394. doi: 10.1146/annurev-pathol-051217-111018
Gutierrez C, Karni RJ, Naqvi S, Aldrich MB, Zhu B, Morrow JR, Sevick-Muraca EM, Rasmussen JC. head and neck lymphedema: treatment response to single and multiple sessions of advanced pneumatic compression therapy. Otolaryngol Head Neck Surg 2019 160, 622-626. doi: 10.1177/0194599818823180
Jessen NA, Munk ASF, Lundgaard I, Nedergaard M. The glymphatic system--a beginner’s guide. Neurochem Res 2015 40, 2583-2599. doi: 10.1007/s11064-015-1581-6
