A guest blog post by Catherine Seo, Ph.D. and Leslyn Keith, OTD, CLT-LANA. This is a 6-minute read.
Lipedema is a little known and generally misdiagnosed fat disorder, primarily in women, resulting in localized painful fat in the lower body including thighs, hips, and in some cases the upper arms. Left untreated or unmanaged, it progresses and can worsen leading to lymphedema and immobility. Lipedema affects as many as 17 million women in the U.S. and 350 million women worldwide.1, 2 It’s commonly confused with obesity, edema, lymphedema, and other health conditions. Typically, onset or exacerbation accompanies hormonal upheavals such as puberty, pregnancy, and perimenopause.
Lipedema’s relationship to obesity is complex. In this BLOG post, we will take a closer look at why lipedema is often confused with simple obesity, what events trigger the condition, how it is distinguished from lymphedema, what defines the stages and types of lipedema, as well as current treatments found to be promising for longer term care and management.
What is Lipedema?
Though lipedema is often unique to each patient based on type, stage, and other comorbidities, generally lipedema presents as a disproportionate distribution of fat creating a smaller upper body compared to a relatively larger lower body. These patients report futile attempts to manage their weight, despite heroic efforts with diet and exercise. Nothing seems to work long-term to reduce weight, pain, and swelling. They feel hopeless that it will ever get resolved. Ultimately the patient’s interactions with their healthcare providers are disappointing at best and traumatic at worst. They are simply not believed.
Healthcare providers respond from anti-fat biases. Since body size and weight have significant impact on perception, even in those cases where there might be underlying medical conditions, there is still the tendency on the part of the healthcare providers to judge and respond when a patient presents either overweight or obese. Healthcare providers often mischaracterize lipedema as obesity and thus as mainly a behavioral problem demonstrating a strong weight bias. It is all too common for the patient with lipedema to be shamed, blamed and told by their healthcare provider that whatever the presenting problem, the underlying cause is behavioral and controllable and that “they are over-eating and under-exercising.”
What Triggers Lipedema?
Lipedema is thought to be hormone-related, occurring almost exclusively in women and at times of hormonal change. Triggers include:
- Puberty
- Pregnancy
- Perimenopause/menopause
- Gynecological surgery or trauma
It could be debated that lipedema actually begins much earlier than most women recognize in their own bodies. For example, a woman might begin to develop the condition shortly after the onset of menarche but the full impact may not be felt until she experiences the body changes that come with pregnancy or menopause.
Lipedema vs. Lymphedema
Lipedema is often confused with and misdiagnosed as lymphedema. These conditions must be differentiated in order to understand and successfully treat the disorder. Although both lipedema and lymphedema have a lymphatic component, there are distinct physiological characteristics that distinguish them from one another. Lipedema is primarily a fat-based disorder while lymphedema is primarily a fluid-based disorder.
These conditions have a relationship to one another, however. Advanced stage lipedema may develop a component of lymphedema due to leaky lymphatic vessels and impaired fluid transport while advanced stage lymphedema may develop excess fat when lymph stasis promotes adipogenesis. Adipogenesis is the cellular differentiation within which pre-adipoctyes become adipocytes, also known as lipocytes or fat cells.
Key diagnostic points to consider:
- Lipedema is bilateral and symmetrical. Lymphedema can be unilateral, but if bilateral the legs are not symmetrical.
- Edema associated with lipedema is non-pitting and the feet are not affected, while lymphedema may have pitting edema and generally includes the feet.
- Cellulitis (painful bacterial skin infection) is rare in lipedema, but can be common in lymphedema.
For more detailed information, refer to Differential Diagnosis Chart provided by the Lipedema Project.
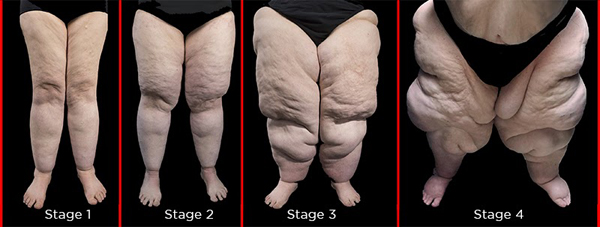
The Stages of Lipedema
Stage 1
In stage one the skin surface can be smooth with enlarging subcutaneous fat tissue (just under the skin and between skin and muscle). There can be swelling that comes and goes depending on various circumstances like nutrition intake and weather conditions. There can be cuffs at the ankles.
Stage 2
In stage two the skin surface is uneven with indentations. There can be the development of nodules in the subcutaneous fat tissue feeling like “beans in a bag,” and in some cases with lipomas (benign fatty tumors). There is a visible “dimpling” of the skin. There can be increasing tenderness and pain. There can be cuffs at the ankles.
Stage 3
In stage three the skin surface increasingly indents with deformations caused by fat growth. There can be large masses of skin and fat that create folds and overhangs especially at the hips, thighs, and knees. Ankle cuffs are present. When lymphedema develops, there can be subcutaneous tissue thickening and a honeycomb appearance to the tissue due to fluid buildup in subcutaneous fat. Pain and tenderness can worsen considerably during this stage with increasing immobility.
Stage 4
In stage four the progression of lipedema advances to include a significant compromise of the lymphatic system and resulting lymphedema. This stage is referred to as LipoLymphedema. There can be debilitating “lobules” of skin and fat, typically on the medial thighs and knees, that significantly limit mobility. Swelling can be persistent. Typically there are profuse cuffs at the ankles.
The Types of Lipedema
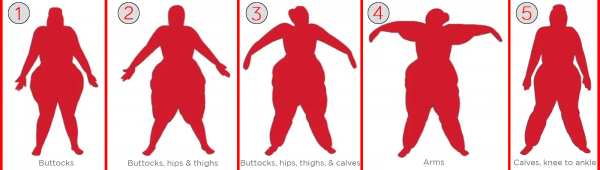 There are five types of lipedema, which are divided according to the region or regions of the body primarily affected.
There are five types of lipedema, which are divided according to the region or regions of the body primarily affected.
Type 1: Buttocks
Fat deposition is mainly concentrated in the buttocks with accumulation sometimes occurring in “saddlebag” formation.
Type 2: Buttocks, Hips, & Thighs
Fat deposition is concentrated in the buttocks, hips, and thighs to the knees. The calves and ankles are unaffected.
Type 3: Buttocks, Hips, Thighs, & Calves
Fat deposition is concentrated in the hips and buttocks, down through the thighs, and into the calves to the ankles. There is often but not always a cuff at the ankles. The feet are spared.
Type 4: Upper Arms
Fat deposition is concentrated in the upper arms. Type 4 accompanies Type 3 in some but not all cases.
Type 5: Calves, Knee to Ankle
Fat deposition is concentrated in the calves from the knees to the ankles sparing the feet. There is often but not always a cuff at the ankles.
Pain and Bruising With Lipedema
While pain often accompanies lipedema, each person can experience pain in a unique way. One woman’s level of pain may be very different from another woman in the same stage of lipedema, and even the locations of pain vary. Not all women with lipedema experience pain. Pain levels might change to becoming more or less painful over time. Those who experience pain report that it occurs primarily in the areas of increased fat deposition, generally between the hips and ankles.
There is also easy bruising with minimal or barely perceptible trauma thought to be the result of capillary fragility and increased permeability. It’s common to see black and blue bruises along the thighs and calves of those with lipedema.
Holistic Approach for Self-Management
Because the experience of lipedema may be unique and all-encompassing for each woman, we strongly believe that a holistic and individualized approach to treatment is required for the best outcomes. A personal protocol for management can be developed by exploring five principal domains: physical, mental/psychological, emotional, spiritual and social.
Physical: This domain includes management of physical symptoms and manifestations of lipedema including pain, swelling, fibrosis, bruising, and fat deposition as well as other secondary consequences such as reduced strength, endurance and mobility. Effective treatment should incorporate nutrition and complete decongestive therapy (manual lymph drainage, compression therapy and movement/exercise). Women are counseled to adopt a ketogenic diet adapted for lipedema and their own unique needs and preferences.3, 4 Complementary treatments investigated may include vibration, cupping, and Epsom salt baths.5, 6, 7
Mental/Psychological: Lipedema affects all aspects of a woman's sense of self-identity, especially in light of the ubiquitous weight bias in our culture. The mental self-chatter and psychological impact can be detrimental to developing a sense of self-nurturance. Interventions can include cultivating Psychological Flexibility, Self-Compassion and broadening Social Connection. Focus on and change to mental self-judgment, criticism and blame can alleviate the internal self-hatred often reported and replace it with acceptance and self-advocacy.
Emotional: The emotional impact of lipedema with its physical disfigurement and functional limitations can be confusing and debilitating. Since self-blame is reported as the most constant issue, a gentle and methodological approach to emotional release can help to transform one’s daily experience. Developing a way of identifying the feelings and emotions that influence all aspects of our lives and decision-making allows for a pathway to acceptance and peace with one’s circumstances.
Spiritual: We have reviewed the many ways in which lipedema is painful across several domains, physical, mental, and emotional. While “Pain is inevitable, suffering is optional.” We support the cultivation of self-compassion and mindfulness, both contributing to a spiritual dimensionality. Self compassion is a deep awareness of our own suffering and being mindful of what we are going through. We are able to notice that this is a part of natural human suffering and that we can relieve it. We cultivate awareness of moments of choice to discover ways to accept what can at times feel overwhelming and out of control. In these moments, we can experience an inner shift. Quiet time, meditation, and other mindfulness practices support the development of self-compassion and deepening spiritual growth.
Social: Most with lipedema feel alone in their struggle with a disease that seems to have no diagnosis or help. They are not being heard or seen or fundamentally understood, often by family and friends, and most definitely in the healthcare setting. Research suggests that connection can be healing. When we feel connected, bodily inflammatory processes change at a physiological level. Three kinds of interactions build closer connections with others. First, vulnerability leads to acceptance. Second, self-disclosing leads to being heard and understood. Finally, asking for what you need leads to reciprocity in relationship with others. These actions create authentic connection. Doing this in community creates safety, a sense of belonging, and willingness to heal. Community leads to better mental and physical health. Helen Keller said, “Alone we can do so little, together we can do so much.”
Lipedema: Challenging And Treatable
The journey of lipedema is challenging and confusing. Most women who have undiagnosed lipedema “know” something is not right but are told again and again by their healthcare providers that it’s their fault, and to stop eating and to start exercising. With a lipedema diagnosis comes mixed feelings. On the one hand, a sense of relief that there is a condition with a definition and a pathophysiology. On the other hand, the conventional belief is that nothing can be done and lipedema will progress to eventual immobility.
We now know that there is a pathway to managing and living well with lipedema. Self-education is at the forefront along with a holistic approach to developing a protocol for self-management. Nutrition based in a ketogenic way of eating has helped many women lose weight, eliminate or diminish pain and swelling, and regain mobility. Cultivation of self-nurturance, self-compassion, and building of community connections worldwide has made a difference in individual and collective knowledge and overall quality of life.
As a lipedema community, we continue to spread awareness about lipedema, eliminate the stigma attached to it, and open a world of possibility for new treatments in the future.
About the authors
Catherine Seo, Ph.D. is Founder & Director of Lipedema Simplified, Founder & Board Member at The Lipedema Project, Inc., course director for MasterClass: Beyond Lipedema and a professor of psychology. She produced and directed the documentary, The Disease They Call FAT, and was one of the co-authors of the book, Lipedema-The Disease They call FAT: An Overview for Clinicians. Catherine's research focuses on empowering women who experience the distortions of body image and the role of nutrition for treating lipedema. She holds a doctorate in Psychology with a concentration in Media. She has lipedema, lymphedema, and has struggled with obesity. Catherine brings knowledge, compassion, and humor to living with a chronic condition.
Leslyn Keith, OTD, CLT-LANA has a Clinical Doctorate in Occupational Therapy with an emphasis on lymphedema and obesity. She was certified as a Lymphedema Therapist in 2000 and became LANA-certified in 2001. Dr. Keith has started four lymphedema therapy programs in California including two in private practice. In addition to treating lymphedema and other lymphatic disorders, she currently researches, consults, and lectures on lymphedema, lipedema, and obesity internationally. She is Board President for The Lipedema Project, Inc. and an instructor for Klose Training and Consulting.
___
Citations:
1. Fife CE, Maus EA, Carter MJ. Lipedema: a frequently misdiagnosed and misunderstood
fatty deposition syndrome. Adv Skin Wound Care. 2010;23(2),81-92. doi: 10.1097/01.
ASW.0000363503.92360.91.
2. Földi M, Földi E. Lipedema. In: Földi M, Földi E, eds. Földi’s Textbook of Lymphology: For Physicians and Lymphedema Therapists. 2nd ed. Munich, Germany: Urban & Fischer; 2007; 417-427.
3. Sørlie, V. (2019). Lipodiet: Effect of a low-carbohydrate high fat-diet on pain and quality of life in patients with lipedema [Master Thesis]. University of Oslo.
4. Gershuni, V. M., Yan, S. L., & Medici, V. (2018). Nutritional Ketosis for Weight Management and Reversal of Metabolic Syndrome. Current Nutrition Reports, 7(3), 97–106. https://doi.org/10.1007/s13668-018-0235-0
5. Rainer Schneider (2020) Low-frequency vibrotherapy considerably improves the effectiveness of manual lymphatic drainage (MLD) in patients with lipedema: A two-armed, randomized, controlled pragmatic trial, Physiotherapy Theory and Practice, 36:1, 63-70, DOI: 10.1080/09593985.2018.1479474
6. Vivian, T. (2019) An overview of lipo-lymphoedema with co-morbid obesity and an example of management, Wound Healing Southern Africa, Volume 12 Number 2, 2019, p. 10 - 14.
7. Ashforth, K. (2019) Understanding Fibrosis in Lipedema: Inflamed Subcutaneous Adipose Tissue (SAT), and Nodules. https://lymphaticnetwork.org/news-events/understanding-fibrosis-in-lipedema-inflamed-subcutaneous-adipose-tissue-sat