A guest blog post by Dr. Andrea Brennan, OTR/L, CLT-LANA, WCC.
Thinking Lymphatically
This article, the second in our three-part series, explains why the existing approach to treating edema and lymphedema is often incomplete, with cutting-edge information just beginning to enter mainstream education. Click to read the first article in this series, which introduces this new research.
It all starts with the English physiologist Ernest Starling in the early 1900s. Starling taught us a wealth of information about microvascular fluid exchange. While Starling was brilliant, he didn’t have the advantage of using modern electron microscopy. Today we know about an important anatomical structure Starling never saw: the glycocalyx.
In this article, we’ll take a closer look at this revolution in understanding fluid regulation and what it means for your patient care. As you read on, keep in mind our theme and one of my personal mottos: “Think lymphatically.”
Fluid Exchange and Starling’s Principle
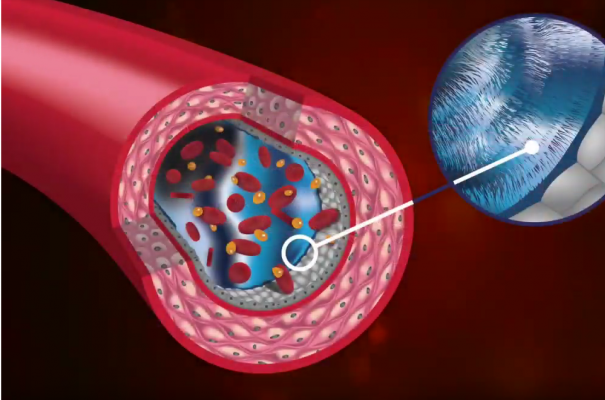
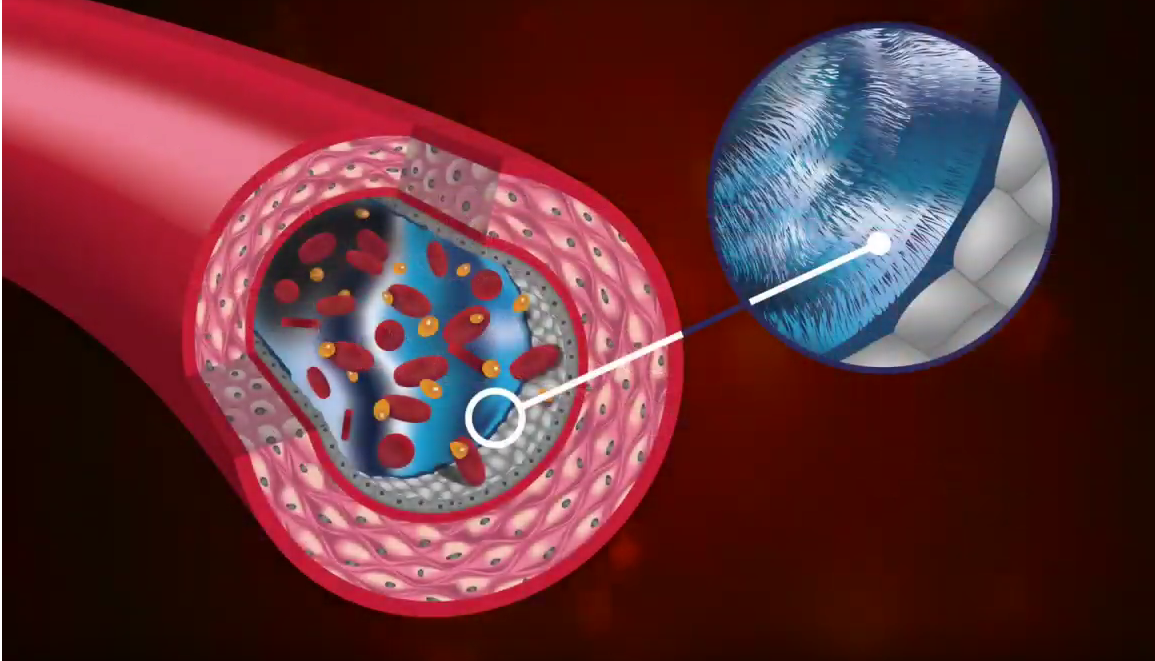
First, let’s review the basics of microvascular fluid exchange. The four main components of microcirculation are capillaries, tissue channels, proteolytic cells (or macrophages) and the initial lymphatics. Everything we’re discussing here is happening right here, at the cellular level.
During microvascular fluid exchange, the capillaries - which are full of holes and fenestrations - allow fluid, nutrients and debris to leave the bloodstream. The fluid, nutrients and debris enter the tissue channels, which are full of macrophages, collagen, protein; everything your body needs to stay healthy and debris, once the body has used them.
Some macrophages reside in the tissue channels, working to break down the large particles of debris so they are small enough to enter the lymphatic system. All of this cellular debris must enter the lymphatic system. Where else could it go?
Pressure and Osmotic Asymmetry
That’s the central question behind Starling’s research and research into microvascular fluid exchange: When pressure builds, what happens?
It’s all about pressure. Think of a garden hose. You turn it on, and the water tries to move from the area of high pressure to the area of lower pressure. This is called osmotic asymmetry - an imbalance in pressure that will always try to balance out. If you add a balloon to the end of the garden hose, the balloon will swell up with nowhere for the fluid to go.
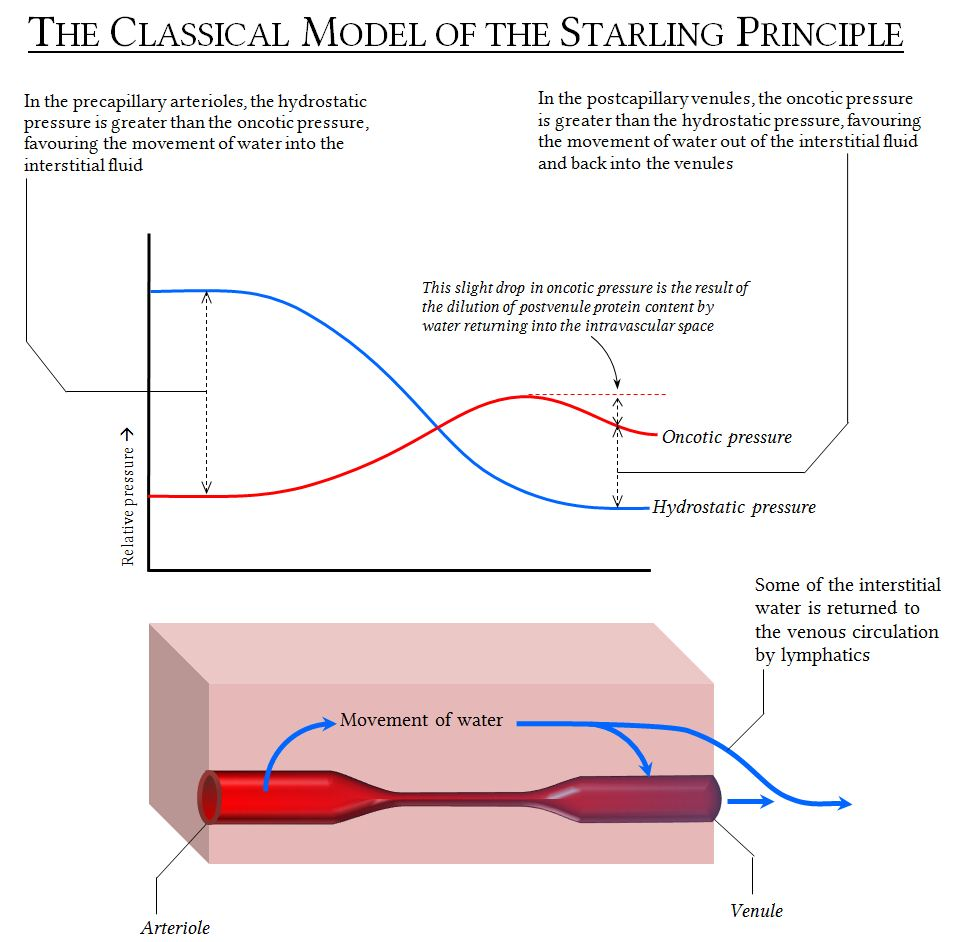
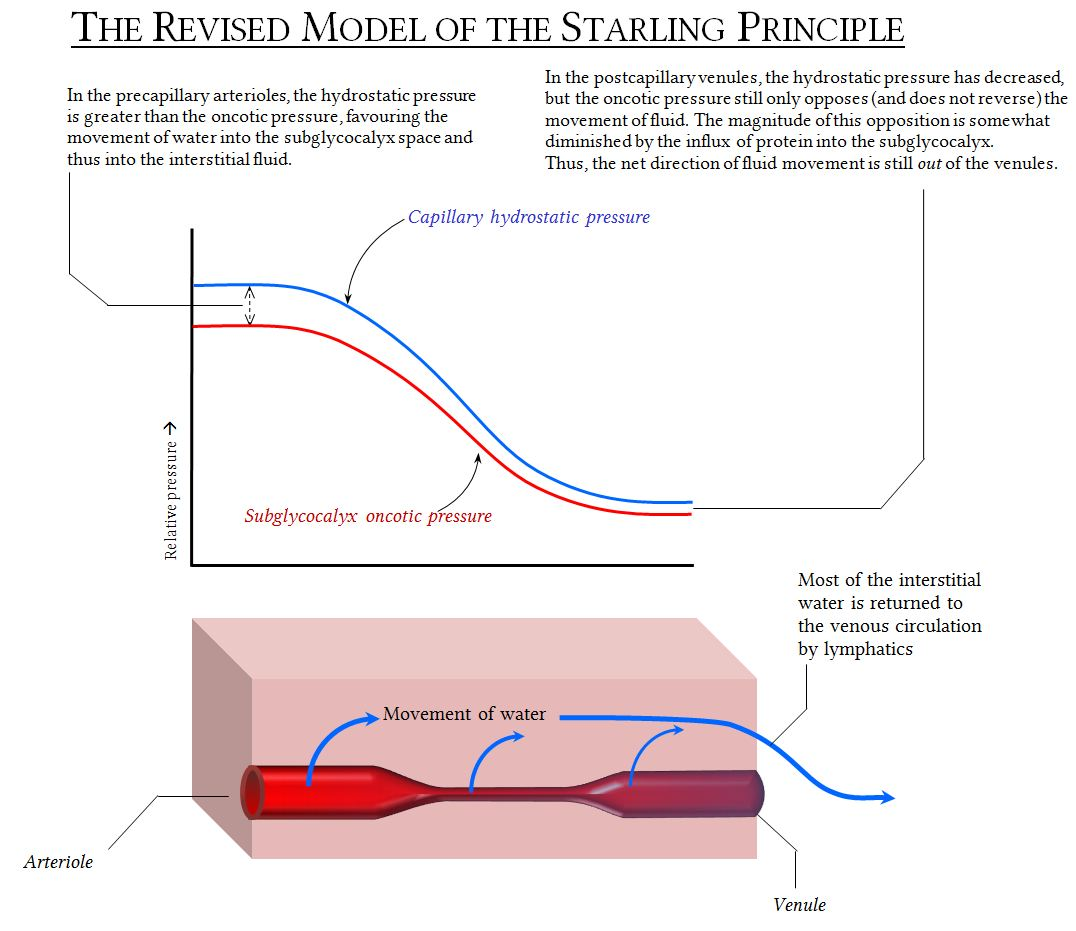
Image source: https://www.derangedphysiology.com
Starling understood pressure at the microvascular level. He theorized that the capillaries are semi-permeable - that, due to the pressure, fluid can move freely across the capillary wall to deliver cellular nutrients and remove debris.
Starling has been applauded for his brilliance, but he never knew that his theory was missing an important component: the endothelial glycocalyx. New research by J.R. Levick and C.C. Michel found there is a lining in the capillary wall called the endothelial glycocalyx. These hairlike structures create an exclusion zone where permeability is reduced. This results in a different tissue pressure measurement. It does not change his equation.
What We Learned From Levick and Michel
Levick and Michel challenged the idea of simple filtration. They helped provide an answer to that important question: Where does the fluid go?
Levick and Michel’s revolutionary work showed fluid crossing from the arterial end of the capillary into the interstitium doesn’t flow back into the capillary at the venous end. This is because the glycocalyx is hydrophobic which changes the pressures and resists fluid from being reabsorbed into the capillary.
Fluid can’t go back into the venous side, because the glycocalyx is opposing the reabsorption into the capillary. The lymphatic system becomes the low pressure outlet for this fluid, cellular debris and nutrients to exit the interstitium.
This gives us a new understanding of what’s happening in the initial lymphatics. Under normal circumstances, 100% of cellular debris, fluids and nutrients must exit into the lymphatic system. The fluid which is entering the lymphatic system is now what is considered to be “lymphatic fluid.”
The Goldilocks Effect on the Lymphatic System
Here we have the Goldilocks effect: too much, too little, and just right. Too much fluid, the patient has edema. Too little fluid, the patient is dehydrated.
The lymphatic system is tasked with preserving equilibrium and keeping fluid balanced. The primary functions of the lymphatic system are to collect and transport tissue fluids, return cellular debris, and break it all down so it can go back into the cardiovascular system. It also digests fats and provides immunological benefits.
While doing all of this, the lymphatics are operating under two main concepts: lymphatic load, or how much fluid is in the lymphatic vessel at any given time, and transport capacity, or how much flow there is per unit of time.
In a normal situation, fluid goes into the lymphatics, they do their work, it goes into the pre-collectors, collectors, lymph nodes, and trunks into the circulatory system all cleansed and ready to go. But if there is an impairment - like too much load, or a broken system - it leads to lymphatic system failure.
There are three main types of lymphatic system failure:
Dynamic insufficiency. There is an increased lymphatic load on a healthy lymphatic system. An example is congestive heart failure. There’s so much fluid, because of the heart problem, that there’s too much fluid for a healthy lymphatic system to manage.
Mechanical insufficiency. There is a normal amount of fluid, but an impaired transport capacity. An example of this is someone who with ovarian cancer undergoes an inguinal node dissection. The node has been removed, and now you have a normal load but the system is no longer intact.
Combined insufficiency. This is an increased load on a damaged lymphatic system. For example, someone has a burn and the initial lymphatics have burned away. For immunological response, the body wants to send fluid to areas that were burned - but now you have a combined insufficiency.
Lymphatic system failure is a serious medical condition for our patients, who often struggle to cope with its impact. If affects their overall health, mental well-being, and quality of life.
Sometimes, edema and lymphedema patients attempt to seek out proper medical treatment for months or years without resolution. It’s a frustrating process for them. Before reaching you, they likely have seen other doctors who thought, “I can’t help this patient.”
Implications for Patient Care
As medical providers, we must update our understanding of the lymphatic system and lymphedema treatment. Our new understanding of osmotic asymmetry, fluid pressure, and the glycocalyx has important clinical implications for our patients.
Here are some key takeaways:
- We must find a way to facilitate lymphatic drainage so there is no stasis fluid in the interstitial area.
- Edema, left unchecked, will eventually become lymphedema.
- A primary consideration for patient treatment should be improving lymphatic flow.
- Because of the pressures and fluid flows involved, external compression is very important.
In my practice, I have seen chronic and stubborn cases where I first wondered, “Is there anything I can do for this patient?” However, with the right kind of therapy, we can make huge improvements - amazing transformations, really - that give every patient a better quality of life.




Used with permission
Next up in the Think Lymphatically Series, we’ll look at complementary treatment modalities that ensure every lymphedema patient receives the best care possible.
About The Author
Dr. Andrea Brennan, OTD, OTR/L, CLT-LANA, CI-CS, WCC holds a clinical doctorate in occupational therapy with a specialty in lymphedema practice management. She has been in the field for more than 35 years and has spent the past 20 years specializing in lymphedema diagnosis and treatment.